Edited in 10/2021 by Consultant Neurosurgeon Mr Al-Mahfoudh
Following your investigations and consultation with your spinal surgeon, the possibility of you undergoing lumbar spinal interbody fusion has been discussed with you. This is an operation where the intervertebral disc, the structure between the bones of the spine (vertebrae), is removed and the space fused with a bone graft.
The healthy intervertebral disc acts as both a spacer and a shock absorber and is composed of two parts: a soft gel-like middle (nucleus pulposus) surrounded by a tougher fibrous wall (annulus fibrosus).
Overhead view of an intervertebral disc (Simplified)
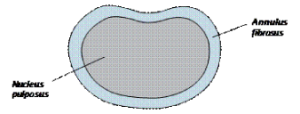
Sometimes the intervertebral discs can lose their flexibility, elasticity and shock absorbing characteristics and the tough layer of ligaments that surrounds the disc may weaken and no longer be able to contain the gel-like substance in the centre. This disc degeneration can cause inflammation in the surrounding area and some of these discs can be a source of continuing back pain and pain in the thighs and buttocks, stiffness, muscle tightness and tenderness. This is known as discogenic pain (pain arising from the disc).
MRI scans may show changes that are due to the natural aging process of the spine and almost everyone will have such changes in their middle age, but this does not necessarily indicate disease. Diagnosis is made after listening carefully to a patient’s symptoms and carrying out a physical examination. Sometimes diagnosis is made following a discography investigation.
Treatment varies depending on the severity of the condition. Most patients only require treatment such as physiotherapy and medication, combined with some lifestyle changes. For patients whose pain does not settle with treatment, surgery may be necessary.
Surgery for lower back pain caused by degenerative disc disease is only considered an option for patients who:
• Have not had sufficient pain relief from extensive non-surgical treatment (such as physiotherapy, medications and pain management programmes) for at least a year;
• Have ongoing lower back pain that limits their ability to perform everyday activities at work or at home; or
• Have received a diagnosis that a specific disc is the pain generator and other possible causes of the lower back pain have been considered and ruled out.
The decision to have a lumbar interbody spinal fusion operation to treat lower back pain caused by degenerative disc disease is a very personal one. For the most part, degenerative disc disease is a non-progressive type of back condition and for the majority of people their symptoms will improve over time (up to ten years). Patients need to carefully consider the risks and possible complications along with the potential benefits of surgery, as well as consider the full range of alternatives to interbody fusion surgery.
Technically, there is a wide variety of surgical procedures that can be performed to fuse the spine, including different cages or spacers (hollow blocks) to insert into the disc space with a bone graft. The approach to the spine can also vary but in this case will be from the front, through the abdomen, by anterior lumbar interbody fusion (ALIF).
Anterior lumbar interbody fusion (ALIF)
Once the diagnosis of degenerative disc disease and the decision to undergo spinal interbody fusion have been made, the goal is then to obtain a solid fusion and stop the movement at that level.
The operation
The operation is performed under general anaesthetic, so you are fully asleep. First, an incision is made through the abdomen. The abdominal contents lay inside a large sack (peritoneum) that can be retracted (moved to the side), allowing the surgeon access to the front of the spine without actually entering the abdomen.
The large blood vessels (aorta, common iliac artery and vena cava) that lie over the front of the spine are carefully moved aside. Sometimes surgery is performed in conjunction with a vascular surgeon, who will mobilise the blood vessels if there are any concerns or difficulty with this.
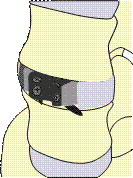
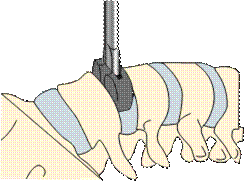
After the blood vessels have been moved aside, a ‘window’ is cut in the anterior ligament and fibrous wall of the disc (annulus fibrosus), retaining as much of it as possible to provide stability for the cage. The disc material (nucleus pulposus) is then removed and the cage, containing bone graft, is placed in the space created. Some cages require screwing into the vertebral body above and below them. Your own bone will, over time, grow into the bone graft.
There are several techniques to get the bone graft needed for spinal fusion:
- patient’s own bone (autograft bone). This is usually taken through an incision over the ileac crest (pelvis);
- donor bone (allograft bone). This eliminates the need to use your own bone. The donor bone graft acts as a calcium scaffolding which your own bone grows into and eventually replaces; or
- artificial bone (bone substitutes).
In the past, patient’s own bone was more commonly used. This can result in complications including chronic pain from the bone graft site, infection and pelvic fractures, so for the most part, artificial bone is now used.
Diagram of cage placement
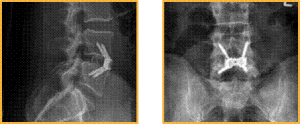
X-rays showing ALIF cage in place, side and front views
Risks and complications
As with any form of surgery, there are risks and complications associated with this procedure.
These can include:
- Damage to the large blood vessels which may result in excessive blood loss. This is reported as happening in up to 15 out of 100 cases, although it is less common in the hands of an experienced spine or vascular surgeon. Usually small tears in the vessels can be controlled reasonably simply, though there remains the very small risk of catastrophic bleeding that could, in extremely rare circumstances, lead to death.
- Superficial wound infections may result in up to 4 out of 100 cases. These are often easily treated with a course of antibiotics.
- Deep wound infections may result in fewer than 1 out of 100 cases. These can be more difficult to treat with antibiotics alone and sometimes patients require more surgery to clean out the infected tissue. This risk may increase for people who have diabetes, reduced immune systems or are taking steroids.
- Blood clots (thromboses) in the deep veins of the legs (DVT) or lungs (PE). This occurs when the blood in the large veins of the leg forms blood clots and may cause the leg to swell and become painful and warm to the touch. Although rare, if not treated, this could be a fatal condition if the blood clot travels from the legs to the lungs, cutting off the blood supply to a portion of the lung. It is reported as happening in fewer than 1 in 700 cases. There are many ways to reduce the risk of blood clots forming. The most effective is to get moving as soon as possible after your operation. Walk regularly as soon as you are able to, both in hospital and when you return home. Perform the leg exercises illustrated in the ‘Preventing Blood Clots’ leaflet and keep well hydrated by drinking plenty of water. Ladies are also advised to stop taking any contraceptive which contains the hormone oestrogen four weeks before surgery, as taking these during spinal surgery can increase the chances of developing a blood clot.
Additionally, we suggest that you remain wearing your anti-embolism stocking (TED stockings) which will be given to you on the ward on your surgery date, for 7 days’ post-operatively. This may be adjusted for a longer/shorter duration if you are not fully mobile or mobilising fully sooner. Your surgeon may give you specific guidance.
- Sympathetic nerve There are small nerves directly over the disc space which can be damaged during surgery. These nerves are responsible for many involuntary organ functions, including the heart rate, peristalsis (gut movement), kidney function and, in men, the ability to ejaculate. If these nerves are damaged it can cause problems including:
- Retrograde ejaculation (men only). This is a condition where the valve that causes the ejaculate to be expelled outward during intercourse does not work and the ejaculate takes the path of least resistance, which is up into the bladder. The sensation remains largely the same and this condition does not cause impotence (the inability to have an erection) but it can unfortunately make conception very difficult. This is reported
in fewer than 1 in 100 cases and can resolve over time (a few months to a year).
- Warm leg. This sensation is felt in just one leg, the same side as the surgery has been performed. This can resolve over time but may be a permanent sensation.
- Paralytic ileus. This is a condition where there is an interruption of the normal bowel contraction and the bowel temporarily ‘goes to sleep’. It can be a common side effect of abdominal surgery or nerve damage in this type of surgery. Symptoms include constipation and bloating and occasionally vomiting. Diagnosis can be confirmed by a doctor listening to the abdomen with a stethoscope and hearing no bowel sounds. Food should be avoided until sounds are heard and flatus (gas) passed again. This condition can occur in 11 out of 100 cases.
- Problems with positioning during the operation which might include skin injuries or pressure Special gel mattresses and heel protection is used to minimise this.
- Abdominal muscle weakness/hernia/bowel perforation/intra-abdominal organ injury/bowel perforation.
- Bone graft non-union or lack of solid fusion (pseudoarthrosis). This can occur in up to 5 out of 100 cases. (See note below on factors which can affect fusion.)
- Cage / Implant movement can occur in up to 2 out of 100 cases with 1 out of 100 requiring re-operation. In extremely rare cases, cage movement can cause severe damage and cauda equina syndrome (see red flag symptoms).
It is vital that seek medical attention or attend the emergency department if you develop any red flag symptoms which include the following;
- Numbness around the saddle area (genitals, buttocks, between the legs)
- Urinary difficulties such as poor flow, urgency, retention of urine, loss of sensation when urinating
- Sciatica-like pain in both legs, or weakness in the legs
- Sexual dysfunction or loss of sensation
- Ongoing pain. ALIF surgery is a complex procedure and not all patients get complete relief with this.
- There are also very rare but serious complications that in extreme circumstances might include a stroke, heart attack or other medical or anaesthetic problems.
Factors which may affect spinal fusion and your recovery
There are a number of factors that can negatively impact on a solid fusion following surgery, including:
- smoking;
- obesity;
- diabetes or chronic illnesses;
- malnutrition;
- osteoporosis;
- post-surgery activities (see advise in recreational activities)
- long-term (chronic) steroid use.
Of all these factors, the one that can compromise fusion rate the most is smoking. Nicotine has been shown to be a bone toxin and inhibit the ability of the bone-growing cells in the body (osteoblasts) to grow bone. Patients should make a concerted effort to allow their body the best chance for their bone to heal by not smoking.
What to expect after surgery and going home?
Immediately after the operation you will be taken on your bed to the recovery ward where nurses will regularly monitor your blood pressure and pulse. Oxygen will be given to you through a facemask for a period of time to help you recover from the anaesthetic. You will have an intravenous drip until you are able to drink adequately.
A drain (tube) may be placed near the surgical incision if there has been significant bleeding during the operation or according to your surgeon’s preference/ routine practice. This removes any excess blood or fluid collecting under the wound. The drain will be removed when the drainage has stopped, usually the next day, after surgery.
It is very normal to experience some level of discomfort after the surgery. The nursing and medical staff will help you to control this with appropriate medication. The symptoms in your legs may fluctuate due to increased swelling around the nerves. As the nerves become less irritated and swollen, your leg pain should settle. This can take eight weeks, or longer. Normal feeling and strength in your legs is likely to take a lot longer and is likely to improve slowly over the next months or so. It is important not to suddenly stop taking certain pain relief medication such as morphine or neuropathic medication (gabapentin, pregabalin or amitriptyline). It will be necessary to gradually ‘wean’ yourself off them – your GP can advise you if necessary.
The ward physiotherapist will visit you after the operation to teach you exercises and help you out of bed. They will show you the correct way to move safely. Once you are confident and independently mobile, you will be encouraged to practise climbing stairs with the physiotherapist.
Once stable you will be allowed home, usually 1 – 2 days after surgery.
You will be given anti-embolism compression stockings (TEDs) which you would have work for your surgery, we advise to wear these for 7 days postoperatively whilst you are likely to be least mobile. Your surgeon may give you specific guidance.
Please arrange for a friend or relative to collect you, as driving yourself or taking public transport is not advised in the initial stages of recovery.
Wound care
Options of skin wound closure depends on your surgeon’s preference, and include absorbable sutures (stitches), removable sutures or clips (surgical staples).
If you have removable sutures or clips, you will be seen by a nurse to remove them usually 10–14 days after the operation in the outpatient department.
If you have absorbable sutures, these still may need to be trimmed and will still require a wound check to take place. The ward staff or consultant secretary will inform you of the date for your appointment or if you prefer to make an appointment with your GP practice nurse.
You may shower 48 hours after surgery if you are careful, but you must avoid getting the wound wet. Most dressings used are ‘splash-proof’, but if water gets underneath, it will need to be changed, a simple, dry dressing from a pharmacy is sufficient to use if a new dressing wasn’t provided on discharge, please make an appointment in this instance for a wound check and re-dressing with outpatients’/specialist nurse. Bathing should be avoided for a minimum of two weeks.
Please contact the hospital if you think your wound might be infected. Symptoms could include:
- redness around the wound;
- wound leakage;
- a high temperature or
- Increased pain at wound site
At a later stage once the wound has healed and been checked, if the scar is sensitive to touch, you can start to massage around the scar using an unperfumed cream or oil to encourage normal sensation and healing.
Recreational activities
It is important to keep mobile after surgery. You will find you get stiff if sitting for longer than about 20 minutes, so get up and walk about regularly. Walking outside is fine but again, increase your walking distances gradually.
You will be advised to avoid lifting anything heavy, certainly for the first few weeks but maybe for as long as three months after your operation.
Please check with your consultant when you are able to resume specific activities, such as swimming or running, as the advice could range from between two weeks to three months. A gradual return to sport is then advisable. You should avoid flying for six weeks (and long-haul flights for up to three months). If you are provided with a LSO lumbar brace wear this for the length of time your consultant has advised (usually 6 weeks) when mobilising.
Driving
Normally you will be advised to stop avoid driving for around four weeks (or when you no longer require a brace if you have been provided with one), but this can be adjusted depending on your recovery. Sitting for prolonged periods is not advisable after your surgery, including driving a car.
If you have no altered sensation or weakness in your legs, then you may return to driving when you feel safe to do so but you must be confident to do an emergency stop.
It is advisable not to travel for long distances initially (no longer than 20 minutes), without taking a break to ‘stretch your legs’. Gradually increase your sitting tolerance over 4 – 8 weeks.
Lifting and carrying
Please ask your consultant and take advice from your physiotherapist. You should avoid heavy lifting and carrying for a few months after your surgery.
Follow-up
You will be sent a clinic appointment for 8 – 12 weeks after your surgery. If you have any queries before this appointment, please contact the nurse specialist for your consultant’s team.
If you have any questions about the information in this booklet, please discuss them with the ward nurses or a member of your consultant’s team.
Information in this leaflet is based on research and revised by spinal nurse specialist Helen Vernau on behalf of the BASS Consent and Patient Information Committee. Illustration by Design Services at The Ipswich Hospital NHS Trust. Edited by Consultant Neurosurgeon Mr Al-Mahfoudh .

What is the British Spine Registry (BSR)?
The British Spine Registry aims to collect information about spinal surgery across the UK. This will help us to find out which spinal operations are the most effective and in which patients they work best. This should improve patient care in the future.
The Registry will enable patient outcomes to be assessed using questionnaires. These will allow surgeons to see how much improvement there has been from treatment.
This has worked for hip and knee joint replacements through the National Joint Registry. We need your help to improve spinal surgery in the UK.
What data is collected?
Your personal details allow the BSR to link you to the surgery you have had. They also allow us to link together all the questionnaires you complete. If you need any further spinal surgery in the future, details of previous operations will be available to your surgeon.
Personal details needed by the BSR are your name, gender, date of birth, address, email address and NHS number.
Your personal details are treated as confidential at all times and will be kept secure. This data is controlled by the British Association of Spine Surgeons (BASS) and held outside the NHS. Personal details will be removed before any data analysis is performed, retaining only age and gender. Your personal data and email address will not be available to anyone outside BASS and its secure IT provider. Anonymised data may be released to approved organisations for approved purposes, but a signed agreement will restrict what they can do with the data so patient confidentiality is protected.
Your personal data is very important, as this will allow us to link details of your diagnosis and surgery with any problems or complications after surgery. You may also be asked to complete questionnaires before and after surgery to work out how successful the surgery has been. These will only be possible if we can connect you to the questionnaires through your personal details.
Do I have to give consent?
No, your participation in the BSR is voluntary and whether you consent or not, your medical care will be the same. Your personal details cannot be kept without your consent. This will be obtained either by asking you to physically sign a consent form or electronically sign one through an email link to a questionnaire or at a questionnaire kiosk in the outpatient clinic.
You can withdraw your consent at any time or request access to your data by:
- going to the patient section of the BSR website at www.britishspineregistry.com; or
- writing to us at the BSR centre (see address overleaf). Please state if you are happy for us to keep existing data, but do not want to be contacted, or whether you want your data to be anonymised (so it cannot be identified).
Research
Your consent will allow the BSR to examine details of your diagnosis, surgical procedure, any complications, your outcome after surgery and your questionnaires. These are known as ‘service evaluations’ or ‘audits’.
Operation and patient information, including questionnaires in the BSR, may be used for medical research. The purpose of this research is to improve our understanding and treatment of spinal problems. The majority of our research uses only anonymised information which means it is impossible to identify individuals. From time to time, researchers may wish to gather additional information. In these cases, we would seek your approval before disclosing your contact details.
You do not have to take part in any research study you are invited to take part in and saying no does not affect the care you receive.
All studies using data from the Registry will be recorded on the BSR website at www.britishspineregistry.com
Further information
The BSR website at www.britishspineregistry.com contains more information, including details of any studies and any information obtained through the Registry data.
To contact the BSR, write to: www.britishspineregistry.com
The British Spine Registry
Amplitude Clinical Services
2nd Floor Orchard House
Victoria Square
Droitwich
Worcestershire WR9 8QT