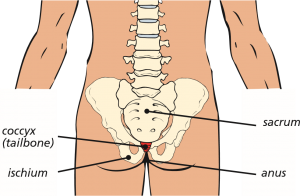
Coccydynia, or coccygeal pain, is the medical term used to describe the pain and tenderness which is felt in the coccyx or tailbone area. The coccyx is the last bone at the bottom of the spine and is joined to the lumbar spine (lower back) by the sacrum.
The pain experienced can often be described as:
- worse when sitting down, particularly when leaning backwards and when getting up and down from a chair
- worse when standing still for long periods
- uncomfortable most of the time, with occasional sharp pains
- worse when opening your bowels or during sexual intercourse
- causing problems with day to day activities, like driving or bending over
- making it difficult to sleep.
Studies have shown that woman are five times more likely than men to develop the condition.
Common causes of coccydynia might include:
- injury or accident, such as a fall backwards
- repeated or prolonged strain on the coccygeal ligaments
(tendinopathy – similar to that of tennis elbow)
- childbirth, particularly after a difficult delivery
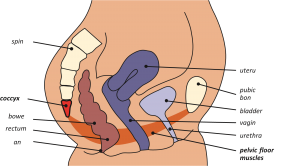
- poor pelvic floor function (pelvic floor muscular structures attach to the coccyx – see diagram overleaf)
- poor posture
- being overweight or experiencing rapid weight loss
- age-related wear and tear.
Less common causes can include the coccyx being too flexible (hypermobility) or too rigid and very rarely, infection or cancer.
Although coccydynia can result from an injury to the coccyx or by straining the surrounding ligaments, sometimes no obvious reason or cause for the condition can be found.
Very few people with coccydynia need medical treatment, as 9 out of 10 people get better spontaneously after a few weeks.
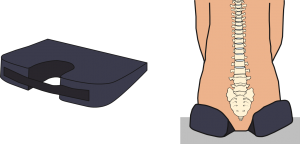
Simple self-help measures which can help to relieve the pain include:
- avoiding sitting for prolonged periods of time or by using a special coccygeal cushion (see diagram below)
- taking non-steroidal anti-inflammatory (NSAID) pain relief medication, such as ibuprofen
- applying hot or cold packs to the lower back region
- physiotherapy exercises, particularly pelvic floor exercises, stretching or massage may also be helpful.
Position of pelvic floor (females)
If the symptoms are severe and ongoing and have not responded to self-help treatment, an injection of anti-inflammatory medicine direct to the source of irritation and / or manipulation of the coccyx can be beneficial and provide excellent pain relief. The injection consists of local anaesthetic which reduces the pain in the short term and a steroid, which will reduce the inflammation in the surrounding area.
About the procedure
The procedure is usually carried out using a combination of sedation (so the patient is asleep) and local anaesthetic, although a general anaesthetic is sometimes advised. You will be asked to lie down on a couch on your stomach or side. The skin is cleaned with antiseptic solution. A radiograph (X-ray) is then used to guide placement of a needle into the coccyx and surrounding ligaments. A small volume of corticosteroid and/or local anaesthetic is then injected. If required, the surgeon may at this stage, insert a gloved finger into the rectum (back passage), to enable manipulation of the coccyx. The injection usually only takes a few minutes to carry out.
Usually patients are just admitted for day case surgery (no overnight stay) as a rapid recovery from any sedation / anaesthesia is expected. Be aware that the local anaesthetic can cause some temporary numbness for a few hours after the injection. Once the numbness has worn off, it is not uncommon for the pain to return, occasionally slightly worse than before, until the corticosteroid takes effect. This can take several days or even a few weeks as steroid injections do take some time to work.
You should continue to take your usual pain relief medication until you begin to feel benefit. It is important not to stop taking certain pain relief medication suddenly, such as, morphine or neuropathic medication (gabapentin, pregabalin or amitriptyline). It will be necessary to gradually ‘wean’ yourself off these medications – your GP can advise you if necessary.
A significant number of patients will experience benefits from a coccygeal injection. However, the duration of benefit is variable and may last a few weeks, several months or years. For a considerable number of patients, the injections can provide excellent pain relief enabling you to continue with physiotherapy, keep active and possibly lose weight if necessary. However, some patients who have had an episode of coccygeal pain are at an increased risk of having a further episode. If an initial injection is helpful a surgeon may offer to repeat the procedure but not usually for about six months.
Risks and complications
Fortunately, there are very few risks associated with coccygeal injections. Very uncommon risks include:
- bleeding. You must inform your consultant if you are taking tablets used to ‘thin the blood’, such as warfarin, rivaroxiban or clopidogrel. It is possible you may need to stop taking these before your injection. If your procedure is scheduled with less than a week’s notice, please check with your consultant or nurse which drugs need to be stopped to prevent this being delayed
- infection. Although this is rare, it is important that the skin at the top of your buttocks is clear of skin conditions like psoriasis, eczema or extreme redness, as these can increase the risk
- facial flushing or (ladies only) interference with the menstrual cycle or post-menopausal bleeding. This can be a temporary side effect of the steroid
- a rise in blood sugar levels for a few days for people who have diabetes
- allergic reactions to the medication.
What to expect in hospital
After the injection, you will be helped back into bed and taken to the recovery ward for a short while, where a nurse will check your blood pressure and pulse. Oxygen may be given to you through a facemask to help you wake up, if required. You will then return to the ward.
Going home
You will normally be allowed home within a couple of hours of having had the injections, once you are up and about.
If you have had intravenous sedation or general anaesthetic, you should not drive for 48 hours and a responsible adult should remain with you overnight. Please arrange for either a friend or relative to collect you from hospital.
Work
You may be advised to take the next day off work, if you had sedation or general anaesthetic, however, you may feel that you need longer if the pain persists. It can take several weeks before the full benefit of the injection takes place. The hospital can give you an off-work certificate or you can ask your GP.
Follow-up
Your surgeon will advise you if you need to attend clinic after your procedure, or how to request a further clinic review if necessary. If you have any queries about the information in this booklet, please discuss them with the ward nurses or a member of your consultant’s team.