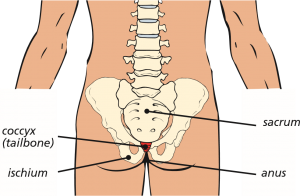
Coccydynia, or coccygeal pain, is the medical term used to describe the pain and tenderness which is felt in the coccyx or tailbone area. The coccyx is the last bone at the bottom of the spine and is joined to the lumbar spine (lower back) by the sacrum. The coccyx consists of two to three bone segments with joints between them.
Coccyx (tailbone) location
The pain experienced can often be described as:
- worse when sitting down, particularly when leaning backwards and when getting up and down from a chair
- worse when standing still for long periods
- uncomfortable most of the time, with occasional sharp pains
- worse when opening your bowels or during sexual intercourse
- causing problems with day to day activities, like driving or bending over
- making it difficult to sleep.
Studies have shown that woman are five times more likely than men to develop the condition.
Common causes of coccydynia might include:
- injury or accident, such as a fall backwards
- repeated or prolonged strain on the coccygeal ligaments
(tendinopathy – similar to that of tennis elbow)
- childbirth, particularly after a difficult delivery
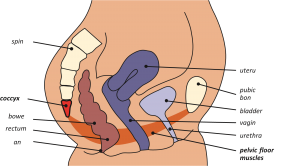
- poor pelvic floor function (pelvic floor muscular structures attach to the coccyx – see diagram overleaf)
- poor posture
- being overweight or experiencing rapid weight loss
- age-related wear and tear.
Less common causes can include the coccyx being too flexible (hypermobility) or too rigid and very rarely, infection or cancer.
Although coccydynia can result from an injury to the coccyx or by straining the surrounding ligaments, sometimes no obvious reason or cause for the condition can be found.
Very few people with coccydynia need medical treatment, as 9 out of 10 people get better spontaneously after a few weeks.
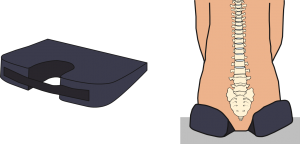
Simple self-help measures which can help to relieve the pain include:
- avoiding sitting for prolonged periods of time or by using a special coccygeal cushion (see diagram below)
- taking non-steroidal anti-inflammatory (NSAID) pain relief medication, such as ibuprofen
- applying hot or cold packs to the lower back region
- physiotherapy exercises, particularly pelvic floor exercises, stretching or massage may also be helpful.
Position of pelvic floor (females)
If the symptoms are severe and ongoing and have not decreased naturally (with time) or improved by self-help technique’s and image-guided steroid injections, then your surgeon may offer you the surgical removal of the coccyx (coccygectomy). However, this is only ever considered as a last resort when all other treatments have been tried, often on more than one occasion.
Most surgeons are reluctant to perform surgical removal of the coccyx for coccydynia, as the success rate for relieving the pain may be only 50% (up to 5 out of 10 cases).
Some recent studies, however, have shown that the success rates may improve, when only specific patients for the procedure are selected. Their selection criteria might include:
- only patients who have had history of an injury to the coccyx
- only patients who have had some pain relief from corticosteroid injections (even if only temporary)
- and / or only patients who have abnormal movement of the coccyx.
The nature of spinal surgery is not a ‘cure’ but is aimed to provide benefit with a good percentage improvement and relief of symptoms. Continued pain can persist, even with a technically successful operation. Good relief from pain following coccygectomy surgery may occur in 50% of cases (up to 5 out of 10 people) or more, depending on the circumstances. This is not usually felt immediately but over a period of time, often several months.
The operation
The operation is commonly called a coccygectomy and involves the surgical removal of either all or part of the coccyx. How much of the coccyx is removed, is decided by your surgeon depending on your situation, for example, the joint(s) of the coccyx can be damaged following a trauma, leaving the lower segment(s) only loosely attached. In this situation, your surgeon may decide to remove only the mobile part of the coccyx. The expected outcomes from each technique is however, very similar.
Coccygectomy
This is performed through an incision at the top of the buttock crease. The skin and soft fat tissue are held apart (retracted) to enable the surgeon to locate the coccyx. Once exposed, the coccyx is gently held and lifted up, carefully dividing it from its surrounding tendinous attachments, either using a scalpel, or by surgical diathermy (a technique which passes an electrical current to burn and cut tissue). Extreme care is required due to the close proximity of the rectum (bowel) under the coccyx bone. Once fully divided, the coccyx can be removed.
Complications
As with any form of surgery, there are risks and complications associated with it. These include:
- persistent pain. It is not uncommon for patients to experience increased pain for several weeks after the operation, especially when sitting down or opening their bowels. It may take between three months up to a year, before the potential benefits of the surgery are effective. However, continued pain after this time may still occur and is one of the biggest risks of surgical removal of the coccyx. Patients may endure a long healing process and still not gain any pain relief after this recovery time
- infection and wound healing problems. Due to the close proximity of the anus and rectum (bowel) to the coccyx, there is a greater risk of infection and wound healing problems after surgery. The bowel contains a large variety of bacteria and extreme vigilance with hygiene, especially after opening the bowels is necessary, until the wound is fully healed. It is also important to avoid constipation and straining when opening your bowels. Taking regular laxatives, especially if taking pain relief medication such as morphine or codeine, will be necessary to avoid this. Wound infections may occur in up to 10 out of 100 cases. These are treated with a course of antibiotics but can cause delayed wound healing. Deep wound infections and delayed wound healing can be more difficult to treat with antibiotics alone and sometimes patients require more surgery to clean out the infected tissue. This risk may increase for people who have diabetes, impaired immune systems or are taking steroids
- injury to the rectum (bowel). Again, due to the proximity to the coccyx, injury to the rectum may occur during surgery. Although this is rare, if it were to happen, immediate formation of a colostomy would be necessary. A colostomy is an operation to divert one end of the bowel through an opening in the tummy (stoma). A pouch is placed over the stoma to collect the stools (poo). This would be temporary to allow time for the bowel to heal. Once healed, another operation to reverse the colostomy, would be performed. Very rarely, a stoma may be required permanently
- prolapse of the pelvic floor. Some of the pelvic floor muscle, tendons and ligaments attach to the coccyx and there have been cases of a prolapse (sagging) of the pelvic floor after surgery. This is a loss of support to the uterus (womb) (women only), bladder and bowel and may cause problems with bladder or bowel function, including incontinence or (for women), pain during sexual intercourse. Physiotherapy may be necessary to help with this and minimise the symptoms
- bleeding. You must inform your consultant if you are taking tablets used to ‘thin the blood’, such as warfarin, aspirin, rivaroxaban or clopidogrel. It is likely you will need to stop taking them before your operation as they increase the risk of bleeding. Taking medication like non-steroidal anti-inflammatories (NSAIDs) could also increase your risk of bleeding and your surgeon will advise you if you need to stop taking these before your operation. If your operation is scheduled with only a week’s notice, please check with your consultant or nurse if any medications you take need to be stopped to prevent your surgery being delayed
- blood clots (thromboses) in the deep veins of the legs (DVT) or lungs (PE). These occur when the blood in the large veins of the leg forms blood clots and may cause the leg to swell and become painful and warm to the touch. Although rare, if not treated this could be a fatal condition if the blood clot travels from the leg to the lungs, cutting off the blood supply to a portion of the lung. It is reported as happening in fewer than 1 out of 700 cases. There are many ways to reduce the risk of a blood clot forming. The most effective is to get moving as soon as possible after your operation. Walk regularly as soon as you are able to, both in hospital and when you return home. Perform the leg exercises as shown to you by the physiotherapist and keep well hydrated by drinking plenty of water. Ladies are also advised to stop taking any medication which contains the hormone oestrogen (like the combined contraceptive pill or HRT) four weeks before surgery, as taking this during surgery can increase the chances of developing a blood clot
- problems with positioning during the operation, which might include pressure problems, skin and nerve injuries. Special gel mattresses and operating tables are used to minimise this.
There are also very rare but serious complications that in extreme circumstances might include:
- stroke, heart attack or other medical or anaesthetic problems
- extremely rarely, general anaesthetic fatal complications which have been reported in 1 out of 250,000 cases.
What to expect after surgery and going home
Immediately after the operation you will be taken on your bed to the recovery ward where nurses will regularly monitor your blood pressure and pulse. Oxygen will be given to you through a facemask for a period of time to help you recover from the anaesthetic. You may have an intravenous drip until you are able to drink adequately.
It is very normal to experience increased pain after the surgery. The nursing and medical staff will help you to control this with appropriate medication. It is likely to be painful to sit down for up to a month post operation and continued use of a specialist cushion is often necessary. It may be necessary to take laxatives for a little while after the operation, to soften your stools (poo) and preventing straining when opening your bowels as this could increase the pain and the potential for wound healing problems. Relief from coccygeal pain may take between three months to a year to settle down. It is important not to suddenly stop taking certain pain relief medication, such as morphine, or neuropathic medication (gabapentin, pregabalin or amitriptyline). It will be necessary to gradually ‘wean’ yourself off them – your GP can advise you if necessary.
Once you are comfortable and independently mobile, you will be allowed home, sometimes the same day but usually the day after surgery.
Please arrange for a friend or relative to collect you, as driving yourself or taking public transport is not advised in the initial stages of recovery.
Wound care
Options for skin wound closure depends on your surgeon’s preference, and include absorbable sutures (stitches), removable sutures or clips (surgical staples).
If you have removable sutures or clips, you will be seen by a nurse to remove them usually 10–14 days after the operation in the outpatient department.
If you have absorbable sutures, these still may need to be trimmed and will still require a wound check to take place. The ward staff or consultant secretary will inform you of the date for your appointment or if you are required to make an appointment with your GP practice nurse.
You may shower 48 hours after surgery if you are careful, but you must avoid getting the wound wet. Most dressings used are ‘splash-proof’, but if water gets underneath, it will need to be changed. A simple, dry dressing from a pharmacy is sufficient to use if a new dressing wasn’t provided on discharge, please make an appointment in this instance for a wound check and re-dressing with outpatients’/specialist nurse. Bathing should be avoided for a minimum of two weeks.
Please contact Nuffield hospital if you think your wound might be infected. Symptoms could include:
- redness around the wound;
- wound leakage;
- a high temperature or
- Increased pain at wound site
At a later stage once the wound has healed and been checked, if the scar is sensitive to touch, you can start to massage around the scar using an unperfumed cream or oil to encourage normal sensation and healing.
Driving
Normally you will be advised to avoid driving for at least four weeks after your surgery, this may be adjusted according to your recovery. If you have no wound problems and your pain is improving by this time, you may resume driving, but you must be confident to do an emergency stop. It is advisable not to travel for long distances initially (no longer than 20 minutes), without taking a break. Gradually increase your sitting tolerance over the next 4 – 8 weeks.
Recreational activities
It is important to keep mobile after surgery. You will find you experience pain and stiffness if sitting for longer than about 20 minutes, so get up and walk about regularly. Walking outside is fine but again, increase your walking distances gradually.
Please check with your consultant when you are able to resume specific activities, such as swimming or running, as the advice could range from between four weeks to three months. A gradual return to sport is then advisable. Your surgeon may advise you to avoid flying for six weeks (and long-haul flights for up to three months), because of the increased risk of deep vein thrombosis after surgery.
Work
Returning to work is dependent both on your recovery and your job. Most people are off work for an initial two weeks but if you are in a sitting job you may need up to six weeks or longer. It is always sensible to discuss with your employer if you can return with consideration to be able to stand up frequently or return on reduced hours at first. There is usually nothing to stop you doing computer / office work, as long as you can keep moving about. The hospital will issue you with a fitness to work (off work) certificate or you may ask your GP.
Follow-up
Your surgeon will advise you when you should attend clinic after your operation. If you have any queries before your follow-up date do please contact the nurse specialist or other member of your consultant’s team.
If you have any questions regarding the information in this booklet, please do discuss them with either the ward nurses or a member of your consultant’s team.
Information in this leaflet is based on research and revised by spinal nurse specialist Helen Vernau on behalf of the BASS Consent and Patient Information Committee. Illustration by Design Services at The Ipswich Hospital NHS Trust. Edited by Consultant Neurosurgeon Mr Rafid Al-Mahfoudh and Spinal Clinical Nurse Specialist Sara Crook with permission from BASS to be used at the Nuffield Brighton Hospital.

What is the British Spine Registry (BSR)?
The British Spine Registry aims to collect information about spinal surgery across the UK. This will help us to find out which spinal operations are the most effective and in which patients they work best. This should improve patient care in the future.
The Registry will enable patient outcomes to be assessed using questionnaires. These will allow surgeons to see how much improvement there has been from treatment.
This has worked for hip and knee joint replacements through the National Joint Registry. We need your help to improve spinal surgery in the UK.
What data is collected?
Your personal details allow the BSR to link you to the surgery you have had. They also allow us to link together all the questionnaires you complete. If you need any further spinal surgery in the future, details of previous operations will be available to your surgeon.
Personal details needed by the BSR are your name, gender, date of birth, address, email address and NHS number.
Your personal details are treated as confidential at all times and will be kept secure. This data is controlled by the British Association of Spine Surgeons (BASS) and held outside the NHS. Personal details will be removed before any data analysis is performed, retaining only age and gender. Your personal data and email address will not be available to anyone outside BASS and its secure IT provider. Anonymised data may be released to approved organisations for approved purposes, but a signed agreement will restrict what they can do with the data so patient confidentiality is protected.
Your personal data is very important, as this will allow us to link details of your diagnosis and surgery with any problems or complications after surgery. You may also be asked to complete questionnaires before and after surgery to work out how successful the surgery has been. This will only be possible if we can connect you to the questionnaires through your personal details.
Do I have to give consent?
No, your participation in the BSR is voluntary and whether you consent or not, your medical care will be the same. Your personal details cannot be kept without your consent. This will be obtained either by asking you to physically sign a consent form or electronically sign one through an email link to a questionnaire or at a questionnaire kiosk in the outpatient clinic.
You can withdraw your consent at any time or request access to your data by:
- going to the patient section of the BSR website at www.britishspineregistry.com; or
- writing to us at the BSR centre. Please state if you are happy for us to keep existing data but do not want to be contacted, or whether you want your data to be anonymised (so it cannot be identified).
Research
Your consent will allow the BSR to examine details of your diagnosis, surgical procedure, any complications, your outcome after surgery and your questionnaires. These are known as ‘service evaluations’ or ‘audits’.
Operation and patient information, including questionnaires in the BSR, may be used for medical research. The purpose of this research is to improve our understanding and treatment of spinal problems. The majority of our research uses only anonymised information which means it is impossible to identify individuals. From time to time, researchers may wish to gather additional information. In these cases we would seek your approval before disclosing your contact details. You do not have to take part in any research study you are invited to take part in and saying no does not affect the care you receive.
All studies using data from the Registry will be recorded on the
BSR website at www.britishspineregistry.com
Further information
The BSR website at www.britishspineregistry.com contains more information, including details of any studies and any information obtained through the Registry data.
To contact the BSR, write to:
The British Spine Registry
Amplitude Clinical Services
2nd Floor
Orchard House
Victoria Square
Droitwich
Worcestershire
WR9 8QT