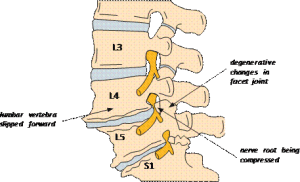
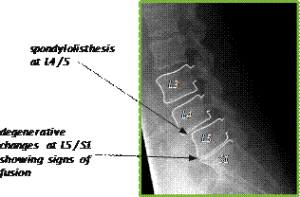
Following your recent investigations and consultation with your spinal surgeon, you have been diagnosed with degenerative lumbar spondylolisthesis.
This is the forward slippage of one lumbar vertebra (bone of the spine) on the vertebra below it. The slippage o ccurs because of wear and tear on the joints that link at the back of the vertebra (facet joints), so much so that the spine is unable to maintain its proper position. The degree of spondylolisthesis may vary from mild to severe. Symptoms may include lower back pain and pain in the thighs and buttocks, stiffness, muscle tightness and tenderness in the area of the slippage.
ccurs because of wear and tear on the joints that link at the back of the vertebra (facet joints), so much so that the spine is unable to maintain its proper position. The degree of spondylolisthesis may vary from mild to severe. Symptoms may include lower back pain and pain in the thighs and buttocks, stiffness, muscle tightness and tenderness in the area of the slippage.
If too much slippage occurs, it can create narrowing of the spinal canal (spinal stenosis).
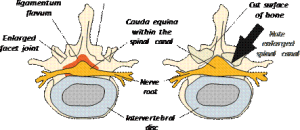
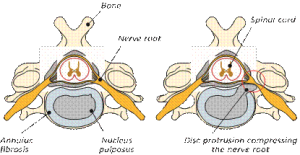
The normal spinal column has a central canal (or passage) through which the spinal nerves pass down. At each side of the vertebral level, spinal nerve roots branch out to each side. The solid spinal cord stops at the top of the lumbar spine (lower back) and from this point the nerves to the bottom and legs pass through the lower canal like a horse’s tail forming the cauda equina. The spinal cord, nerve roots and cauda equina are surrounded by cerebrospinal fluid (CSF) and are all contained within a membrane, or covering, called the dura mater, rather like the thin layer that covers a boiled egg.
The ligamentum flavum is a tough band of elastic tissue (ligament) that connects the vertebrae and provides stability for posture and protection for the dura mater.
There are five bones (vertebra) in the lumbar spine. In between each bone is an intervertebral disc, which acts as both a spacer and a shock absorber. Over time as disc degeneration (wear and tear) occurs, the disc will lose water and height and as such, close down the bony passage (foramen) where the nerve root passes through on leaving the spine.
In spinal stenosis, the spinal nerve roots and / or cauda equina become trapped or compressed by the narrowing of these nerve passages, by arthritic joint swelling and bony overgrowths (osteophytes) which grow into the spinal canal and the bunching up (buckling) of the ligamentum flavum, like an elastic band losing tension or bulging of the intervertebral discs.
Diagram 1 showing spondylolisthesis at L4 / L5
When nerves are compressed they can produce symptoms of pain, numbness and tingling in the legs and felt in the area of the leg that the particular spinal nerve supplies. In rare cases they can produce severe pain and even weakness in the legs, such that the ‘legs don’t work’. In most cases, the symptoms are produced when standing or walking and are relieved by sitting or bending forward, as this can temporarily open up the nerve passages. In rare cases the nerves which control your bladder, bowel and sexual function can be compressed. This is known as cauda equina syndrome (CES) and often requires urgent surgical intervention. Fortunately, immediate spinal surgery is only necessary in a few cases. However, it is vital that seek medical attention or attend the emergency department if you develop any red flag symptoms which include the following;
- Numbness around the saddle area (genitals, buttocks, between the legs)
- Urinary difficulties such as poor flow, urgency, retention of urine, loss of sensation when urinating
- Sciatica-like pain in both legs, or weakness in the legs
- Sexual dysfunction or loss of sensation
Unfortunately, most conservative treatments (manipulation, physiotherapy, medication or injections) are unlikely to be of much long-term benefit, and the symptoms rarely improve permanently without surgery to take the pressure off the nerves (decompression), as well as dealing with the instability of the spine.
The objective of surgery is to remove the material (for example the excess bone and ‘bunched up’ ligament from the back of the spinal canal) to give the nerve roots and / or cauda equina more room. The surgeon will decide whether there is a need to stabilise the spine by using an internal implant system. Sometimes radical decompression surgery can further weaken the spine’s stability, so the exact extent of surgery can only be decided during the procedure.
Below is a cross-sectional (axial) view of the disc, cauda equina, nerve roots and facet joints of the spine. Note the size of the spinal canal after surgical decompression (diagram 3).
The nature of spinal surgery is not to ‘cure’, and it cannot prevent further degeneration of the spine, but is aimed to provide benefit with a good percentage improvement and relief of leg symptoms. Good relief from leg symptoms following decompression surgery usually occurs in approximately 70 – 80% of cases (up to 8 out of 10 people). This is not necessarily felt immediately but over a period of time, often several months. Sometimes however, numbness or weakness can persist, even with a technically successful operation. This can occur when people have more extensive stenosis before they have surgery. Rarely, the surgery may make your symptoms worse than they were before.
The results of the operation are not nearly as reliable for the relief of lower back pain. Much of the back pain experienced comes from arthritis and associated muscular spasms, therefore, decompression surgery cannot eliminate this and it should not be regarded as the main aim of the surgery.
The operation
There are several different techniques when performing an operation to deal with the condition called degenerative spondylolisthesis. Expected outcomes from all methods are very similar and the choice of operation will be decided by the surgeon.
Decompression
Laminectomy and / or laminotomy
This is performed through an incision in the midline of the lower back. The position and length of incision is determined by which levels of the spine and how many nerves are involved. The muscles are then held apart to gain access to the bony arch and roof of the spine (lamina). Next, the surgeon needs to gain entry into the spinal canal by removing some bone, either by cutting away the whole area of lamina (laminectomy) or making a small window in the lamina (laminotomy) with a high-speed burr (like a dentist’s drill). Bone and ligament are removed and often the facet joints, which are directly over the nerve roots, are undercut (trimmed) to relieve the pressure on the nerves and give them a wider passage as they pass out of the spine.
Minimally invasive (tubular) decompression
With this approach, the surgeon attempts to reduce muscle dissection and injury by working through a narrow tube. There may be several small incisions depending on how many nerves are involved.
Stabilisation
Before stabilisation surgery is carried out, several factors are taken into consideration. These include assessing how unstable the spinal segments are, which nerves are involved and how narrow the nerve canal has become. Your surgeon may request a standing x-ray to help assess the need for stabilisation.
Bone graft
This is used to fuse (join together) and stabilise the spine in conjunction with other techniques, which are mentioned below. It is laid between the outer segments of the spine, in between the transverse process (intertransverse region) and your new bone will, over time, grow into the bone graft. This is a biological process over 3 – 6 months, known as spinal fusion. There are several techniques to obtain the bone graft needed for spinal fusion:
- patient’s own bone (autograft bone). The bone that is removed during surgery can be used as a bone graft. If more is needed, for the most part, artificial bone is now used, although it can be taken from the pelvis (iliac crest) if required;
- donor bone (allograft bone). Donor bone graft does not contain living bone cells but acts as calcium scaffolding which your own bone grows into and eventually replaces.
Pedicle screw fixation
This is a system of screws and rods which hold the vertebra together and prevents movement at the segment that is being fused, like an internal scaffolding system. Screws are placed into the part of the vertebra called the pedicle, which go directly from the back of the spine to the front, on both sides, above and below the unstable spinal segment. These screws then act as firm anchor points to which rods can be connected. After the bone graft grows and fuses to the spine (after many months), the rods and screws are no longer needed for stability. However, most surgeons do not recommend removing them except in rare cases.
Side view of pedicle screw, Overhead view of pedicle
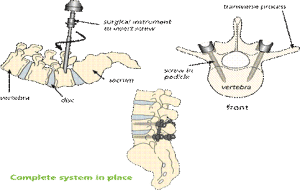
Placement screw in vertebral body
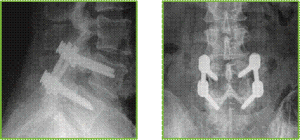
X-rays showing the stabilisation system in place, side and front views
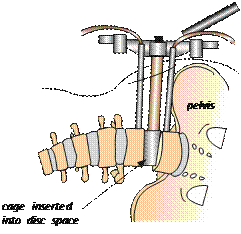
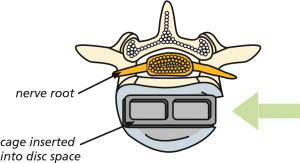
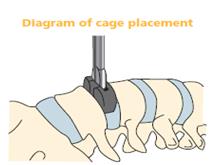
Interbody fusion
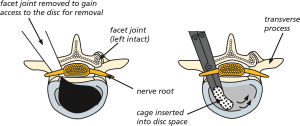
This is a procedure where the surgeon will remove the intervertebral disc, the structure between the bones of the spine (vertebra), and fuse the space with a cage and bone graft. This can enable the surgeon to achieve an all-round (360°) spinal fusion and to increase the height of the interbody space and therefore the bone canal, for the nerve to pass through.
Intervertebral fusion cages
This is like a hollow Lego brick which props up the disc space between the two bones (vertebra). It is a tight fit and gives immediate stability. The cage is different widths, heights and depths to fit your spine exactly. It is made from carbon fibre or titanium metal. They can be filled with bone graft or artificial bone if required and are used in interbody fusion surgery.
The surgical approach (way in) to interbody fusion also varies and can include:
• posterior lumbar interbody fusion (PLIF). The spine is approached from the back and part of the lamina bone and facet joint is removed on both sides to gain access to the disc;
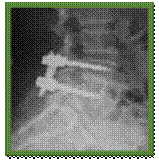
X-rays showing the before and after stabilisation system in place, side and front views
Posterior lumbar interbody fusion (PLIF)
- Transforaminal lumbar interbody fusion (TLIF). The spine is approached again from the back and all of the facet joint is removed on one side to gain access to the disc; and
Transforaminal lumbar interbody fusion (TLIF)
- Extreme lateral interbody fusion (XLIF). The spine is approached from the side of the body, through an incision just above the pelvis. This particular approach to the spine has risks and complications which are specific to it and are listed below the general ones.
Extreme lateral interbody fusion (XLIF) approach
Extreme lateral interbody fusion (XLIF)
Anterior lumber interbody fusion (ALIF)
• The spine is approached from the front (abdomen). The abdomen contents which may lay within a large sac (peritoneum) are retracted (moved to the side)
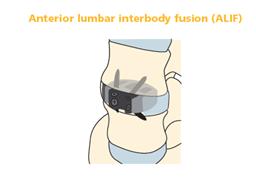
The large blood vessels (aorta, common iliac artery and vena cava) that lie over the front of the spine are carefully moved aside. Sometimes surgery is performed in conjunction with a vascular surgeon, who will mobilise the blood vessels if there are any concerns or difficulty with this
After the blood vessels have been moved aside, a ‘window’ is cut in the anterior ligament and fibrous wall of the disc (annulus fibrosus), retaining as much of it as possible to provide stability for the cage. The disc material (nucleus pulposus) is then removed and the cage, containing bone graft, is placed in the space created. Some cages require screwing into the vertebral body above and below them. Your own bone will, over time, grow into the bone graft.
Risks and complications
As with any form of surgery, there are risks and complications associated with this procedure. Your surgeon may mention different percentages and depending on your individual case.
These can include:
- damage to a nerve root. This occurs in less than 1 out of 100 cases of primary surgery but is much more common in revision or ‘re-do’ surgeries where injury can occur in up to 10 out of 100 cases. If this happens, you may get weakness in the muscles supplied by that particular nerve root and / or numbness, tingling or hypersensitivity in the area of skin it supplies;
- tearing of the outer lining or covering which surrounds the nerve roots (dura). This is reported in fewer than 5 out of 100 cases. It may occur as a result of the bone being very stuck to the lining and tearing it as the bone is lifted off. Again, it is much more common in ‘re-do’ surgery. Usually the hole or tear in the dura is repaired with stitches, a patch or a special glue. If the puncture or hole re-opens you may get cerebrospinal fluid (CSF) leaking from the wound, headaches or, very rarely, meningitis. Although rare, the problems of leakage can persist. This could result in you having to return to theatre to enable the surgeon to revise the repair of the dura but the risk of a second operation being required within a few days or weeks is less than 0.05%;
- recurrent leg pain as a result of scarring;
- problems with positioning during the operation, which might include pressure problems, skin and nerve injuries, and eye complications including, very rarely, blindness. Special gel mattresses and operating tables are used to minimise this;
- Superficial wound infections may occur in up to 4 out of 100 cases. These are often easily treated with a course of antibiotics. Deep wound infections may occur in fewer than 1 out of 100 cases. These can be more difficult to treat with antibiotics alone and sometimes patients require more surgery to clean out the infected tissue. This risk may increase for people who have diabetes, impaired immune systems or are taking steroids;
- blood clots (thromboses) in the deep veins of the legs (DVT) or lungs (PE). These occur when the blood in the large veins of the leg forms blood clots and may cause the leg to swell and become painful and warm to the touch. Although rare, if not treated this could be a fatal condition if the blood clot travels from the leg to the lungs, cutting off the blood supply to a portion of the lung. It is reported as happening in fewer than 1 out of 700 cases. There are many ways to reduce the risk of a blood clot forming. The most effective is to get moving as soon as possible after your operation. Walk regularly as soon as you are able to, both in hospital and when you return home. Perform the leg exercises as shown to you by the physiotherapist and keep well hydrated by drinking plenty of water. Ladies are also advised to stop taking any medication which contains the hormone oestrogen (like the combined contraceptive pill or HRT) four weeks before surgery, as taking this during spinal surgery can increase the chances of developing a blood clot;
- difficulty with screw placement, including injury to the nerves or screw breakage;
- You must inform your consultant if you are taking tablets used to ‘thin the blood’, such as warfarin, aspirin, rivaroxiban or clopidogrel. It is likely you will need to stop taking them before your operation as they increase the risk of bleeding. Taking medication like non-steroidal anti-inflammatories (NSAIDs) could also increase your risk of bleeding and your surgeon will advise you if you need to stop taking these before your operation. If your operation is scheduled with only a week’s notice, please check with your consultant or nurse if any medications you take need to be stopped to prevent your surgery being delayed;
- bone graft non-union or lack of solid fusion (pseudoarthrosis). This can occur in up to 5 out of 100 cases. See below for factors which can affect fusion; and
- although rare, the surgery may make your symptoms worse than before.
- Chest infections. You may need antibiotics and physiotherapy.
There are also very rare but serious complications that in extreme circumstances might include:
- damage to the cauda equina and paralysis (the loss of use of the legs, loss of sensation and loss of control of the bladder and bowel). This can occur through bleeding into the spinal canal after surgery (a haematoma). If an event of this nature were to occur, every effort would be made to reverse the situation by returning to theatre to wash out the haematoma. Sometimes, however, paralysis can occur as a result of damage or reduction of the blood supply of the nerves or spinal cord and this is, unfortunately, not reversible;
- stroke, heart attack or other medical or anaesthetic problems; and
- extremely rarely, death; as a result of damage to major blood vessels or vital organs at the front of the spine, which is reported as happening in 1 out of 10,000 cases; or general anaesthetic fatal complications which have been reported in 1 out of 250,000 cases.
XLIF-specific risks and complications
- Damage of nerves which could result in thigh pain and / or numbness and weakness of the muscles involved with hip flexion, which may be temporary or permanent.
- Abdominal muscle weakness/hernia/bowel perforation/intra-abdominal organ injury/bowel perforation.
ALIF-specific risks and complications
- Damage to the large blood vessels which may result in excessive blood loss. This is reported as happening in up to 15 out of 100 cases, although it is less common in the hands of an experienced spine or vascular surgeon. Usually small tears in the vessels can be controlled reasonably simply, though there remains the very small risk of catastrophic bleeding that could, in extremely rare circumstances, lead to death.
- Sympathetic nerve damage. There are small nerves directly over the disc space which can be damaged during surgery. These nerves are responsible for many involuntary organ functions, including the heart rate, peristalsis (gut movement), kidney function and, in men, the ability to ejaculate. If these nerves are damaged it can cause problems including:
- Retrograde ejaculation (men only). This is a condition where the valve that causes the ejaculate to be expelled outward during intercourse does not work and the ejaculate takes the path of least resistance, which is up into the bladder. The sensation remains largely the same and this condition does not cause impotence (the inability to have an erection) but it can unfortunately make conception very difficult. This is reported in fewer than 1 in 100 cases and can resolve over time (a few months to a year).
- Warm leg. This sensation is felt in just one leg, the same side as the surgery has been performed. This can resolve over time but may be a permanent sensation.
- Paralytic ileus. This is a condition where there is an interruption of the normal bowel contraction and the bowel temporarily ‘goes to sleep’. It can be a common side effect of abdominal surgery or nerve damage in this type of surgery. Symptoms include constipation and bloating and occasionally vomiting. Diagnosis can be confirmed by a doctor listening to the abdomen with a stethoscope and hearing no bowel sounds. Food should be avoided until sounds are heard and flatus (gas) passed again. This condition can occur in 11 out of 100 cases.
- Abdominal muscle weakness/hernia/bowel perforation/intra-abdominal organ injury/bowel perforation.
Factors which may affect spinal fusion and your recovery
There are a number of factors that can negatively impact on a solid fusion following surgery, including:
- smoking;
- diabetes or chronic illness;
- obesity;
- malnutrition;
- osteoporosis;
- post-surgery activities (see note of recreational activities); and
- long-term (chronic) steroid use.
Of all these factors, the one that can compromise fusion rate the most is smoking. Nicotine has been shown to be a bone toxin and it inhibits the ability of the bone-growing cells in the body (osteoblasts) to grow bone. Patients should make a concerted effort to allow their body the best chance for their bone to heal by not smoking, ideally for 2 – 3 months before the operation. Your surgery may be delayed or cancelled if you have not stopped smoking – or having nicotine in another form – beforehand.
What to expect after surgery and going home?
Immediately after the operation you will be taken on your bed to the recovery ward where nurses will regularly monitor your blood pressure and pulse. Oxygen will be given to you through a facemask for a period of time to help you recover from the anaesthetic. You will have an intravenous drip until you are able to drink adequately.
A drain (tube) may be placed near the surgical incision if there has been significant bleeding during the operation or according to your surgeon’s preference/ routine practice. This removes any excess blood or fluid collecting under the wound. The drain will be removed when the drainage has stopped, usually the next day, after surgery.
It is very normal to experience some level of discomfort or back and leg pain after the surgery. The nursing and medical staff will help you to control this with appropriate medication. The symptoms in your legs may fluctuate due to increased swelling around the nerves. As the nerves become less irritated and swollen, your leg pain should settle. This can take eight weeks, or longer. Normal feeling and strength in your legs is likely to take a lot longer and is likely to improve slowly over the next year or so. It is important not to suddenly stop taking certain pain relief medication such as morphine or neuropathic medication (gabapentin, pregabalin or amitriptyline). It will be necessary to gradually ‘wean’ yourself off them – your GP can advise you if necessary.
The ward physiotherapist will visit you after the operation to teach you exercises and help you out of bed. They will show you the correct way to move safely. Once you are confident and independently mobile, you will be encouraged to practise climbing stairs with the physiotherapist.
Once stable you will be allowed home, usually 1 – 2 days after surgery.
Additionally, we suggest that you remain wearing your anti-embolism stocking (TED stockings) which will be given to you on the ward on your surgery date, for 7 days’ post-operatively. This may be adjusted for a longer/shorter duration if you are not fully mobile or mobilising fully sooner.
Please arrange for a friend or relative to collect you, as driving yourself or taking public transport is not advised in the initial stages of recovery.
Wound care
Skin wound closure depends on your surgeon’s preference, and include absorbable sutures (stitches), removable sutures or clips (surgical staples).
If you have removable sutures or clips, you will be seen by a nurse to remove them usually 10–14 days after the operation in the outpatient department.
If you have absorbable sutures, these still may need to be trimmed and will still require a wound check to take place. The ward staff or consultant secretary will inform you of the date for your appointment or if you prefer to make an appointment with your GP practice nurse.
You may shower 48 hours after surgery if you are careful, but you must avoid getting the wound wet. Most dressings used are ‘splash-proof’, but if water gets underneath, it will need to be changed, a simple, dry dressing from a pharmacy is sufficient to use if a new dressing wasn’t provided on discharge, please make an appointment in this instance for a wound check and re-dressing with outpatients’/specialist nurse. Bathing should be avoided for a minimum of two weeks.
Please contact your hospital if you think your wound might be infected. Symptoms could include:
- redness around the wound;
- wound leakage;
- a high temperature or
- Increased pain at wound site
At a later stage once the wound has healed and been checked, if the scar is sensitive to touch, you can start to massage around the scar using an unperfumed cream or oil to encourage normal sensation and healing.
Driving
Normally you will be advised to avoid driving for four weeks (or when you no longer require the brace, if you have been provided with one), depending on your recovery.
If you have no altered sensation or weakness in your legs at that point, then you may resume driving if you feel safe to do so, but you must be confident to do an emergency stop.
It is advisable not to travel for long distances initially (no longer than 20 minutes), without taking a break to ‘stretch your legs’. Gradually increase your sitting tolerance over 4 – 8 weeks.
Recreational activities
It is important to keep mobile after surgery. You will find you get stiff if sitting for longer than about 20 minutes, so get up and walk about regularly. Walking outside is fine but again, increase your walking distances gradually.
You will be advised to avoid lifting anything heavy, certainly for the first few weeks but maybe for as long as three months after your operation.
Please check with your consultant when you are able to resume specific activities, such as swimming or running, as the advice could range from between two weeks to three months. A gradual return to sport is then advisable. You should avoid flying for six weeks (and long-haul flights for up to three months). If you are provided with a LSO lumbar brace wear this for the length of time your consultant has advised (usually 6 weeks) when mobilising.
Work
Returning to work is dependent both on your recovery and your job. Most people are off work for an initial four weeks but if you are in a strenuous job you may need up to six weeks. It is always sensible to discuss with your employer if you can return on ‘light duties’ or reduced hours at first. There is usually nothing to stop you doing computer / office work at an earlier date, as long as you can keep moving about. The hospital will issue you with a fitness to work (off work) certificate or you may ask your GP.
Follow-up
Your surgeon will advise you when you should attend clinic after your operation. If you have any queries before your follow-up date do, please contact the nurse specialist or other member of your consultant’s team.
If you have any questions about the information in this booklet, please discuss them with the ward nurses or a member of your consultant’s team.

What is the British Spine Registry (BSR)?
The British Spine Registry aims to collect information about spinal surgery across the UK. This will help us to find out which spinal operations are the most effective and in which patients they work best. This should improve patient care in the future.
The Registry will enable patient outcomes to be assessed using questionnaires. These will allow surgeons to see how much improvement there has been from treatment.
This has worked for hip and knee joint replacements through the National Joint Registry. We need your help to improve spinal surgery in the UK.
What data is collected?
Your personal details allow the BSR to link you to the surgery you have had. They also allow us to link together all the questionnaires you complete. If you need any further spinal surgery in the future, details of previous operations will be available to your surgeon.
Personal details needed by the BSR are your name, gender, date of birth, address, email address and NHS number.
Your personal details are treated as confidential at all times and will be kept secure. This data is controlled by the British Association of Spine Surgeons (BASS) and held outside the NHS. Personal details will be removed before any data analysis is performed, retaining only age and gender. Your personal data and email address will not be available to anyone outside BASS and its secure IT provider. Anonymised data may be released to approved organisations for approved purposes, but a signed agreement will restrict what they can do with the data so patient confidentiality is protected.
Your personal data is very important, as this will allow us to link details of your diagnosis and surgery with any problems or complications after surgery. You may also be asked to complete questionnaires before and after surgery to work out how successful the surgery has been. These will only be possible if we can connect you to the questionnaires through your personal details.
Do I have to give consent?
No, your participation in the BSR is voluntary and whether you consent or not, your medical care will be the same. Your personal details cannot be kept without your consent. This will be obtained either by asking you to physically sign a consent form or electronically sign one through an email link to a questionnaire or at a questionnaire kiosk in the outpatient clinic.
You can withdraw your consent at any time or request access to your data by:
- going to the patient section of the BSR website at www.britishspineregistry.com; or
- writing to us at the BSR centre (see address overleaf). Please state if you are happy for us to keep existing data, but do not want to be contacted, or whether you want your data to be anonymised (so it cannot be identified).
Research
Your consent will allow the BSR to examine details of your diagnosis, surgical procedure, any complications, your outcome after surgery and your questionnaires. These are known as ‘service evaluations’ or ‘audits’.
Operation and patient information, including questionnaires in the BSR, may be used for medical research. The purpose of this research is to improve our understanding and treatment of spinal problems. The majority of our research uses only anonymised information which means it is impossible to identify individuals. From time to time, researchers may wish to gather additional information. In these cases, we would seek your approval before disclosing your contact details.
You do not have to take part in any research study you are invited to take part in and saying no does not affect the care you receive.
All studies using data from the Registry will be recorded on the BSR website at www.britishspineregistry.com
Further information
The BSR website at www.britishspineregistry.com contains more information, including details of any studies and any information obtained through the Registry data.
To contact the BSR, write to: www.britishspineregistry.com
The British Spine Registry
Amplitude Clinical Services
2nd Floor Orchard House
Victoria Square
Droitwich
Worcestershire WR9 8QT