 Imaging techniques, such as an X-ray or MRI scan, can reveal problems with the lumbar spine such as thinning discs, osteoarthritis or facet joint degeneration (wear and tear).
Imaging techniques, such as an X-ray or MRI scan, can reveal problems with the lumbar spine such as thinning discs, osteoarthritis or facet joint degeneration (wear and tear).
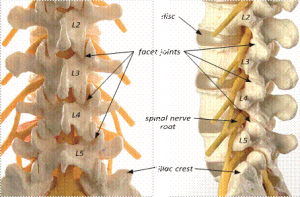
In the lumbar spine, there are five bones (vertebra) and in between each bone is an intervertebral disc which acts as both a spacer and a shock absorber. The bony spine and discs are surrounded by muscles (core muscles) and at the back of each spinal vertebrae is a pair of interlocking and moving connections called facet joints, where some of these muscles join to. These joints slide over each other enabling the spine to bend and twist. Both joint surfaces are coated with a moist cushioning tissue (cartilage). A small capsule surrounds each facet joint and provides a lubricant for the joint and contains nerve fibres that give warning when there is irritation or inflammation.
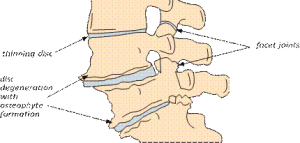
 Over time, the intervertebral discs lose water and their flexibility, elasticity and shock-absorbing characteristics (disc degeneration). As the disc degenerates, it becomes thin and the pressure or load on the facet joints becomes greater. If the muscles surrounding the spine also become weaker, then more stress is placed on the discs and facet joints.
Over time, the intervertebral discs lose water and their flexibility, elasticity and shock-absorbing characteristics (disc degeneration). As the disc degenerates, it becomes thin and the pressure or load on the facet joints becomes greater. If the muscles surrounding the spine also become weaker, then more stress is placed on the discs and facet joints.
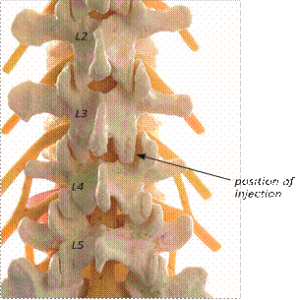
Model of the lumbar spine showing the facet joints and nerve roots.
Diagram showing the degeneration in the lumbar spine
Just like any joint in the body, the facet joints can become inflamed due to the wear and tear on the cartilage surface and resulting arthritis. This can cause pain and stiffness, usually in the lower back, which can radiate (travel) over the hips and into the groins and thighs. This is typically called ‘hands in pocket’ pain because the pain is felt in the area where your hands travel, when putting them into a trouser front pocket. The pain suffered from facet joint degeneration can often be mistaken as a problem with the hip joint, as it can be very similar.
Typically facet joint pain and associated muscle spasms, often referred to as facet syndrome, come and go. People often report increased pain after prolonged periods of inactivity like sleeping, sitting or standing too long. Most people complain that pain is most pronounced first thing in the morning, decreases throughout the day if they are moving about and become worse again later in the evening. Pain can also be brought on by twisting movements of the spine or leaning backwards (extension). Changing your position regularly can improve the symptoms but be careful not to get out of bed or a chair too quickly, as the spinal muscles can spasm and ‘lock’ to prevent joint irritation, causing a sharp pain across the lower back region which seems to prevent you from moving for a short while. This is typically what happens when people say that their ‘back has gone’.
Being overweight will also increase the load on the facet joints and increase the symptoms experienced, so losing weight can help significantly.
If symptoms are prolonged and interfering with day-to-day life, an injection of anti-inflammatory medicine direct to the source of irritation, can be beneficial and provide excellent pain relief. This should be followed a week or so later by an ongoing exercise program to strengthen the core muscles and help reduce the likelihood and severity of pain returning. Injection therapy should not be considered the only treatment for low back pain. Continued rehabilitation and stronger muscles for your own ‘internal corset’ is vital for the future ‘health’ of your spine.
Facet block injections can also be performed as a diagnostic tool to help your specialist understand your condition. If there is pain relief following the injection, even if only temporary, it can confirm that the back pain originates from the facet joints.
About the procedure
The procedure is carried out with either intravenous sedation (so the patient is asleep) or under local anaesthetic injection, to numb the injection site and surrounding area. You will be asked to lie down on the operating table on your stomach, usually with your head facing to one side on a pillow. The skin on the back is cleaned with antiseptic solution. Live X-ray is then used as guidance to direct the needle into the facet joint capsule. A small volume of corticosteroid and / or local anaesthetic is injected. This usually only takes a few minutes to carry out, depending on how many joints are being treated.
Right L3 / 4 facet joint injection (back view)
This procedure is carried out as a day case (no overnight stay) and can lead to a rapid recovery. The local anaesthetic can cause some temporary numbness for a few hours after the injection. Once the numbness has worn off, it is not uncommon for the pain to return, occasionally slightly worse than before, until the corticosteroid takes effect. This can take several days or even a few weeks as anti-inflammatories take some time to reduce the inflammation surrounding the spine.
We monitor for a minimum of 2 hours post procedure if sedation is used. If you have sedation you will be required to be nil by mouth (starved/fasting) 6 hours prior to your procedure. You may however drink water up to two hours prior to your injection. Please keep in mind you will be at the hospital for most of the day.
Usually patients are just admitted for day case surgery as a rapid recovery from any sedation / anaesthetic is expected. Be aware that the local anaesthetic given may cause some temporary leg numbness or weakness for a few hours. You will need to be careful when getting out of bed, that any weakness does not cause your leg to ‘give way’ and for you to fall over.
You should continue to take your usual pain relief medication until you begin to feel the benefit of the corticosteroid. It is important not to stop taking certain pain relief medication suddenly, such as, morphine or neuropathic medication (gabapentin, pregabalin or amitriptyline). After an adequate period of time it will be necessary to gradually ‘wean’ yourself off them – your consultant or GP can advise you if necessary.
Eighty percent of patients will experience significant benefits from these injections. However, the duration of benefit is variable and may last a few weeks, months or years. For a considerable number of patients, the injections can provide excellent pain relief enabling you to continue with physiotherapy, keep active and possibly lose weight if necessary. However, some patients who have had an episode of facet syndrome are at an increased risk of having a further episode. It may be possible to repeat the injections, if the first has been helpful, although not straight away. Most specialists would wait at least six months before repeating them.
If the symptoms have not improved after six weeks or the relief only temporary up to that point, then in certain circumstances, the next stage may be to come back to clinic for further assessment or treatment.
Risks and complications
Fortunately, there are very few risks associated with facet joint injections. Very uncommon risks include:
- You must inform your consultant if you are taking tablets used to ‘thin the blood’, such as warfarin, rivaroxaban, clopidogrel and aspirin. It is likely you will need to stop taking these before your injection. If your procedure is scheduled with less than a week’s notice, please check with your consultant or nurse which drugs need to be stopped to prevent this being delayed
- Although this is rare, it is important that the skin on your back is clear of skin conditions like psoriasis or eczema as these can increase the risk
- facial flushing or, in women, interference with the menstrual cycle or post-menopausal bleeding. This can be a temporary side effect of the steroid
- a rise in blood sugar levels for a few days for people who have diabetes
- a needle injury to the dura (the membrane around the nerves). This is usually apparent at the time of injection and can result in a small leakage of the cerebrospinal fluid (CSF), which can lead to a headache (when standing and walking) for a few days afterwards. If this does occur, you may be advised to lie down for a period of time.
- allergic reactions to the medications or radiographic contrast (dye) used. Serious consideration is necessary for patients who are known to have chronic kidney disease (CKD) as the dye can adversely affect the kidney function, which is rare cases could lead to kidney failure. This dye isn’t used in all cases and many doctors perform facet injections without this dye.
- Risks of sedation. During your sedation your breathing may become slow, this is particularly common in deep sedation, but is a risk whenever sedation is used. Your anaesthetist is skilled in monitoring you and can support your breathing if required. It is very common that your blood pressure may drop by a small amount. It is very common to be left with a small bruise where your cannula was placed. Feeling sick or vomiting is uncommon. There is a small risk of stomach contents going into your lungs therefore it is vital to follow fasting instructions to keep this risk very low. Any allergic reaction to the sedation drugs is very rare. You may be at a higher risk of falling, especially if you are elderly. It is common for sedation to affect your judgement and memory for up to 24 hours.
Sometimes however, it is difficult to place the needle and inject directly into the joint space due to the presence of bony overgrowths. In this situation, the pain relief from the injection may not be quite as effective.
What to expect on the day
Your admission time may be early (i.e. 07:00am) as it is likely that you are part of an operating list in theatres. The reason for this is, so all patient for that day can been seen by the anaesthetist and consultant. This also gives time for a comprehensive admission to the ward and getting changed ready for theatre. However, unavoidable things can happen on the day and they may be a wait. You will walk (if able to) to theatre with a ward nurse and porter to be checked in with the anaesthetist and theatre team.
After the injection, you will be taken to the recovery ward on your bed for a short while, where a nurse will check your blood pressure and pulse. Oxygen may be given to you through a facemask to help you wake up, if you were given sedation. You will then return to the ward. When ready you will be offered a light refreshment before you are discharged home.
Going home
You will normally be allowed home within a couple of hours of having had the injections, once you are up and about.
If you have had intravenous sedation, then you will usually be monitored for around 1-2 hours on the ward depending on your sedation type and how you are feeling.
Please arrange for either a friend or relative to collect you from hospital. If you have had intravenous sedation, you should not drive for 48 hours and a responsible adult should remain with you overnight.
Driving
We advise that you avoid driving for a few days depending on how your symptoms are after your procedure. If you have no altered sensation and weakness in your legs and minimal pain, you may resume driving if you feel safe to do so, but you must be comfortable to do an emergency stop.
Work
You may be advised to take the next day off work, if you had intravenous sedation, however, you may feel that you need longer and if the pain persists. It can take several weeks before the full benefit of the injection takes place. The hospital can give you an off-work certificate, remember to request this during your admission or you can call the ward if you forget alternatively, you can ask your GP.
Follow-up
Your surgeon will advise you when you need to attend clinic after your procedure, or how to request a further clinic review if necessary. If you have any queries about the information in this booklet, please discuss them with the ward nurses or a member of your consultant’s team.