Introduction
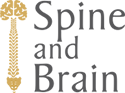
The sacroiliac (SI) joints are located at the base of the spine, between the sacrum (the triangular bone at the bottom of the spine) and the iliac bones of the pelvis. They act as shock absorbers, reducing stress on the pelvis and spine, and transferring the load of the upper body to the lower body during standing and walking.
Like any joint in the body, the SI joints can become painful due to arthritis, wear and tear, or abnormal movement (either too much or too little). This can cause pain directly over the joint, across the lower back, or radiating into the buttocks, groin, or down the back of the legs. These symptoms are often mistaken for hip or lumbar spine problems, as they can be very similar.
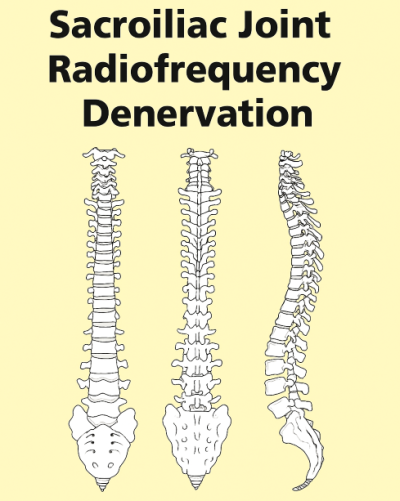
Radiofrequency denervation of the sacroiliac joint is a treatment designed to provide longer-lasting pain relief. It works by using radiofrequency energy to heat and interrupt the small nerves that carry pain signals from the sacroiliac joints. This reduces the ability of the joint to transmit pain messages to the brain.
About the Procedure
The procedure is usually performed under local anaesthetic, although intravenous sedation may be given to help you relax or sleep through the procedure. You will lie on your stomach on the operating table. The skin over your lower back is cleaned with antiseptic solution.
Using X-ray (fluoroscopy) guidance, the doctor positions specialised radiofrequency needles alongside the small nerves around the sacroiliac joint. Once the needles are correctly placed, test stimulation may be carried out to confirm accuracy. A small dose of local anaesthetic is then given, followed by the application of radiofrequency energy. This heats the nerve for 60–90 seconds, temporarily disrupting its ability to carry pain signals. Several nerves around each joint may need to be treated during the same session.
The whole procedure usually takes 30–60 minutes depending on how many nerves are treated. It is a day case procedure, so you will usually go home the same day.
Pre-operative assessment
A member of the pre-operative team will contact you to discuss important details and assess your fitness for surgery. They will ask about your medical history, any current medications, and allergies, as well as answer any questions you may have about the procedure. This step ensures that the surgical team has all the necessary information to plan your care safely. In some cases, you may also be invited to attend a pre-assessment clinic, where additional checks can be carried out to confirm that you are ready for the procedure.
Fasting
It is essential to follow the fasting instructions before your procedure. You must stop eating solid food 6 hours before the operation. Clear fluids such as water, black tea, or black coffee (without milk) can be consumed up to 2 hours before your procedure. However, nothing should be eaten or drunk in the final 2 hours before the procedure. These guidelines are very important to reduce the risk of complications related to sedation or anaesthesia.
Risks and Complications
Sacroiliac joint radiofrequency denervation is a safe and commonly performed procedure, but risks include:
• Local bruising or soreness at the injection site
• Temporary numbness or weakness in the back, buttocks, or legs
• Tingling or altered sensation around the treated area (usually temporary)
• Rarely, infection or bleeding at the needle site
• Very rarely, persistent nerve pain or weakness
• Side effects of sedation: drowsiness, nausea, low blood pressure, slowed breathing, or temporary memory impairment (all carefully monitored)
If you are taking blood-thinning medicines (such as warfarin, rivaroxaban, clopidogrel or aspirin), you must inform your consultant as these may need to be stopped before the procedure.
What to Expect on the Day
You may be admitted early so that your anaesthetist and consultant can see you before the procedure. You will be taken to theatre, where the radiofrequency denervation will be performed. Afterwards, you will be monitored in the recovery ward while your pulse and blood pressure are checked. If sedation was given, oxygen may be provided while you wake up.
Most patients are discharged the same day, once they are able to walk safely and feel comfortable.
Going Home
You will normally be discharged within 1–2 hours of the procedure. If sedation was used, you must not drive for 48 hours and a responsible adult should stay with you overnight.
Some discomfort, muscle spasm, or bruising around the treated joint may last for a few days before the long-term benefit develops.
It is important to continue your usual pain medications until you feel the benefit of the injection. Do not stop strong painkillers (such as morphine, gabapentin, pregabalin or amitriptyline) suddenly – your GP or consultant will advise you on tapering them if necessary.
Driving
Do not drive until you feel confident that you can perform an emergency stop safely. If you have persistent numbness, weakness, or significant pain, you should wait until these symptoms settle. Most patients can drive within a few days.
Work
If you had sedation, you should take at least the following day off work. Some patients may need longer depending on their recovery. A medical certificate can be provided by the hospital if required.
Follow-up
Your consultant will arrange a follow-up appointment. The pain relief from radiofrequency denervation can last many months or even years, although the nerves may regenerate over time. If this happens, the procedure can be repeated if it was helpful previously.
Approximately 70–80% of patients experience significant benefit, which allows them to stay active, reduce medication, and continue with physiotherapy or exercise programs.
—————
For further information / contact us
Mr Al-Mahfoudh’s PA
07501 703075
secretary@spineandbrain.co.uk
Pre-operative team at Spire Gatwick
01293 306 122
gphpre-assessment@spirehealthcare.com
Pre-operative team at Spire Montefiore
01273 829 350
montefioreadmissionspsc@spirehealthcare.com