Following your recent investigations and consultation with your spinal surgeon, your scans have revealed that you have one or more fractured vertebrae (bones of the spine).
This could have been caused by osteoporosis, injury to your back or less commonly cancer, as these can weaken a bone’s structure. Osteoporosis (meaning porous bone) is a disease that results in a loss of normal bone density, mass and strength, which can result in the bones becoming more susceptible to breaking.
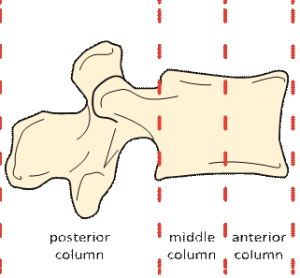
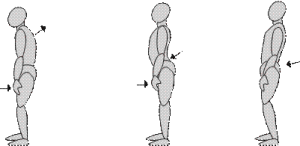
When a vertebral body fractures, the bone squashes down (compresses) and the usual rectangular shape is permanently altered. Typically, this occurs at the front edge of the vertebra (anterior column) and will give the bone a wedge like appearance (anterior wedge compression fracture).
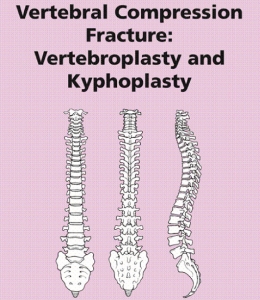
Diagram showing how the normal vertebra is defined in sections
This type of fracture of the vertebral bone can cause extreme back pain along with other symptoms, such as losing height, spinal deformity or a ‘hunched’ appearance (kyphosis) because of the increased forward tilt of the spine. These appearances can be more pronounced the more bones that are involved.
In certain circumstances if the condition worsens, it can lead to collapse or narrowing of the spinal canal and pressure on the spinal nerves. This can cause pain, numbness, increased sensitivity or even weakness of the muscles in the area supplied by that particular spinal nerve.
Vertebroplasty and kyphoplasty are surgical procedures where bone cement is injected into a fractured vertebra to stabilise it and reduce the pain. 
Vertebral body compression fractures are usually treated by conservative measures, such as strong medication, bed rest and / or bracing until the pain settles. Vertebroplasty or kyphoplasty can now be offered to patients where these treatments have been difficult to tolerate and for patients who:
- Have uncontrolled pain
- have conditions that limit their ability to tolerate bed rest or the taking of strong medication
- are elderly or frail and are likely to have impaired bone healing following a fracture
- have a vertebral compression fracture due to a malignant tumour
- suffer from osteoporosis due to long-term steroid treatment or a metabolic disorder.
 There are, however, limitations to what this type of treatment can achieve. Some of the pain experienced is due to muscular spasms resulting from the spinal deformity or pain from the lower back joints (facet joints).
There are, however, limitations to what this type of treatment can achieve. Some of the pain experienced is due to muscular spasms resulting from the spinal deformity or pain from the lower back joints (facet joints).
This can happen when people following injury, adopt a change of posture by leaning backwards to try and ‘reverse’ the forward tilt (thoracic kyphosis) of the spine. This can increase the load on the joints, resulting in inflammation and pain.
The procedure
The procedure is usually carried out under a general anaesthetic, so you are fully asleep, lying on your stomach. The skin on your back is cleaned with antiseptic solution and a small incision is made to one or both sides of the midline. There will be a small incision for each vertebra requiring treatment.
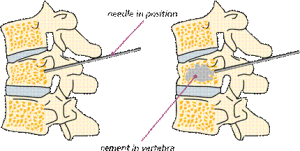
A hollow needle is then passed down through the muscle into a bony passage (pedicle), which goes from the back of the spine to the front of the vertebral body. Live X-ray is used as guidance to direct the needle into this area. Several X-rays are taken from the side and back views, to ensure that the needle is through the pedicle and into the vertebra.
For vertebroplasty, the liquid cement is injected into the vertebra through the hollow needle. Several x-rays are taken to show the cements movement into the vertebra. The cement becomes hard in minutes.
Diagram showing needle placement and insertion of cement
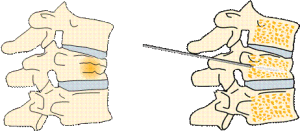
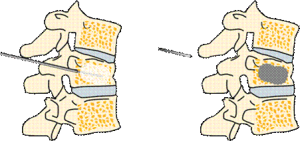
During kyphoplasty, a balloon is first inserted into the fractured vertebrae through the hollow needle to create a cavity or space. The balloon is then removed, and the liquid cement is injected into the cavity it created. Several X-rays are taken to show the cements movement into the vertebra. The cement becomes hard in minutes.
fractured vertebra, ballon inserted into uertebra
show the cements movement into the vertebra. The cement becomes hard in minutes.
medical cement inside vertebra, ballon inserted into uertebra
Risks and complications
As with any form of surgery, there are risks and complications associated with this procedure.
These can include:
- leakage of the cement outside the vertebral body, which could rarely cause thermal (heat) and pressure problems in the spinal canal. This in turn could cause neurological (nerve) problems including, in extreme cases, paralysis. X-rays are taken throughout the procedure to observe for signs of leakage. The surgeon can stop injecting the cement immediately, if this occurs, therefore minimising the risk of nerve damage
- rarely travelling of particles of cement, air, bone marrow fat or tumour, into the blood vessels causing a blockage (embolisation). This could in extreme cases put stress on the lungs, heart or other organs
- very rarely cement sensitivity, which could cause the heart to have irregular beats. This could, in extreme cases, bring on a cardiac arrest (the heart to stop) and death
- Superficial wound infections may occur in 2 – 4% of cases (up to 4 out of 100 people). These are often easily treated with a course of antibiotics. Deep wound infections may occur in < 1% of cases (fewer than 1 out of 100 people). These can be more difficult to treat with antibiotics alone and sometimes patients require more surgery to clean out the infected tissue. This risk may increase for people who have diabetes, reduced immune systems or are taking steroids
- You must inform your consultant if you are taking tablets used to thin the blood, such as warfarin, aspirin, rivaroxaban or clopidogrel. It is likely you will need to stop taking them before your operation as they increase the risk of bleeding. If your operation is scheduled with less than a week’s notice, please check with your consultant or nurse which drugs need to be stopped to prevent your surgery being delayed
- the increased strength in the vertebra following vertebroplasty, may increase the chances of the adjacent vertebral body wedging in the future
- problems with positioning during the operation which might include pressure problems, skin and nerve injuries and eye complications including, very rarely, blindness. A special gel mattress and protection is used to minimise this
- extremely rarely, death; as a result of damage to major blood vessels or vital organs at the front of the spine, which is reported as happening in 1 out of 10,000 cases
- general anaesthetic fatal complications which have been reported in 1 out of 250,000 cases.
- Chest infections – you may require antibiotic or physiotherapy
What to expect in hospital?
Immediately after the procedure you will be taken to the recovery ward, where nurses will monitor your blood pressure and pulse. Oxygen may be given to you through a facemask to help you wake up after the anaesthetic. Once back on the ward, if you have some discomfort, the nursing staff will give you appropriate medication to help control it. When you are fully awake and comfortable, you will be allowed to get out of bed. This may be the same day.
Going home
If you do not require any further treatment for your condition, you will normally be allowed home the following day, when you and your physiotherapist and consultant are happy with your mobility.
Please arrange for a friend or relative to collect you, as driving yourself or taking public transport is not advised for 48 hours after the anaesthetic.
Driving
We advise that you may need to avoid driving for a few days depending on how your symptoms are after your procedure. If you have no altered sensation and weakness in your legs and minimal pain, you may resume driving if you feel safe to do so, but you must be comfortable to do an emergency stop.
Work
Returning to work is dependent on both your recovery and your job. You will need to be off work for at least 48 hours or maybe longer if discomfort persists and with consultant advise. The hospital will issue you with a fitness to work (sick) certificate, you can request this whilst you are in hospital or can call the ward if you have been discharged, furthermore you can request this from your GP.
Follow up
Your specialist will advise you whether you when you should attend clinic after your operation. If you have any queries before this appointment, please contact the nurse specialist or other member of your consultant’s team.
If you have any questions regarding the above, please discuss them with either the ward nurses or a member of your consultant’s team.

What is the British Spine Registry (BSR)?
The British Spine Registry aims to collect information about spinal surgery across the UK. This will help us to find out which spinal operations are the most effective and in which patients they work best. This should improve patient care in the future.
The Registry will enable patient outcomes to be assessed using questionnaires. These will allow surgeons to see how much improvement there has been from treatment.
This has worked for hip and knee joint replacements through the National Joint Registry. We need your help to improve spinal surgery in the UK.
What data is collected?
Your personal details allow the BSR to link you to the surgery you have had. They also allow us to link together all the questionnaires you complete. If you need any further spinal surgery in the future, details of previous operations will be available to your surgeon.
Personal details needed by the BSR are your name, gender, date of birth, address, email address and NHS number.
Your personal details are treated as confidential at all times and will be kept secure. This data is controlled by the British Association of Spine Surgeons (BASS) and held outside the NHS. Personal details will be removed before any data analysis is performed, retaining only age and gender. Your personal data and email address will not be available to anyone outside BASS and its secure IT provider. Anonymised data may be released to approved organisations for approved purposes, but a signed agreement will restrict what they can do with the data so patient confidentiality is protected.
Your personal data is very important, as this will allow us to link details of your diagnosis and surgery with any problems or complications after surgery. You may also be asked to complete questionnaires before and after surgery to work out how successful the surgery has been. This will only be possible if we can connect you to the questionnaires through your personal details.
Do I have to give consent?
No, your participation in the BSR is voluntary and whether you consent or not your medical care will be the same. Your personal details cannot be kept without your consent. This will be obtained either by asking you to physically sign a consent form or electronically sign one through an email link to a questionnaire or at a questionnaire kiosk in the outpatient clinic.
You can withdraw your consent at any time or request access to your data by:
- going to the patient section of the BSR website at britishspineregistry.com; or
- writing to us at the BSR centre. Please state if you are happy for us to keep existing data but do not want to be contacted, or whether you want your data to be anonymised (so it cannot be identified).
Research
Your consent will allow the BSR to examine details of your diagnosis, surgical procedure, any complications, your outcome after surgery and your questionnaires. These are known as ‘service evaluations’ or ‘audits’.
Operation and patient information, including questionnaires in the BSR, may be used for medical research. The purpose of this research is to improve our understanding and treatment of spinal problems. The majority of our research uses only anonymised information which means it is impossible to identify individuals.
From time to time, researchers may wish to gather additional information. In these cases, we would seek your approval before disclosing your contact details. You do not have to take part in any research study you are invited to take part in and saying no does not affect the care you receive. All studies using data from the Registry will be recorded on the BSR website at britishspineregistry.com
Further information
The BSR website at britishspineregistry.com contains more information, including details of any studies and any information obtained through the Registry data.
To contact the BSR, write to: britishspineregistry.com
The British Spine Registry
Amplitude Clinical Services
2nd Floor
Orchard House
Victoria Square
Droitwich
Worcestershire
WR9